Managing vs. Treating Urinary Incontinence (UI):
Bladder Leaks Don’t Have to Rule Your Life
Doctors and physiotherapists call it a “silent epidemic.” It can interfere with day-to-day life, intimacy, and travel plans, and it can steal away self-confidence.
We’re talking about urinary incontinence in women, and it’s more common than you might think—at least one in three women will deal with it at some point.1
What Is Urinary Incontinence?
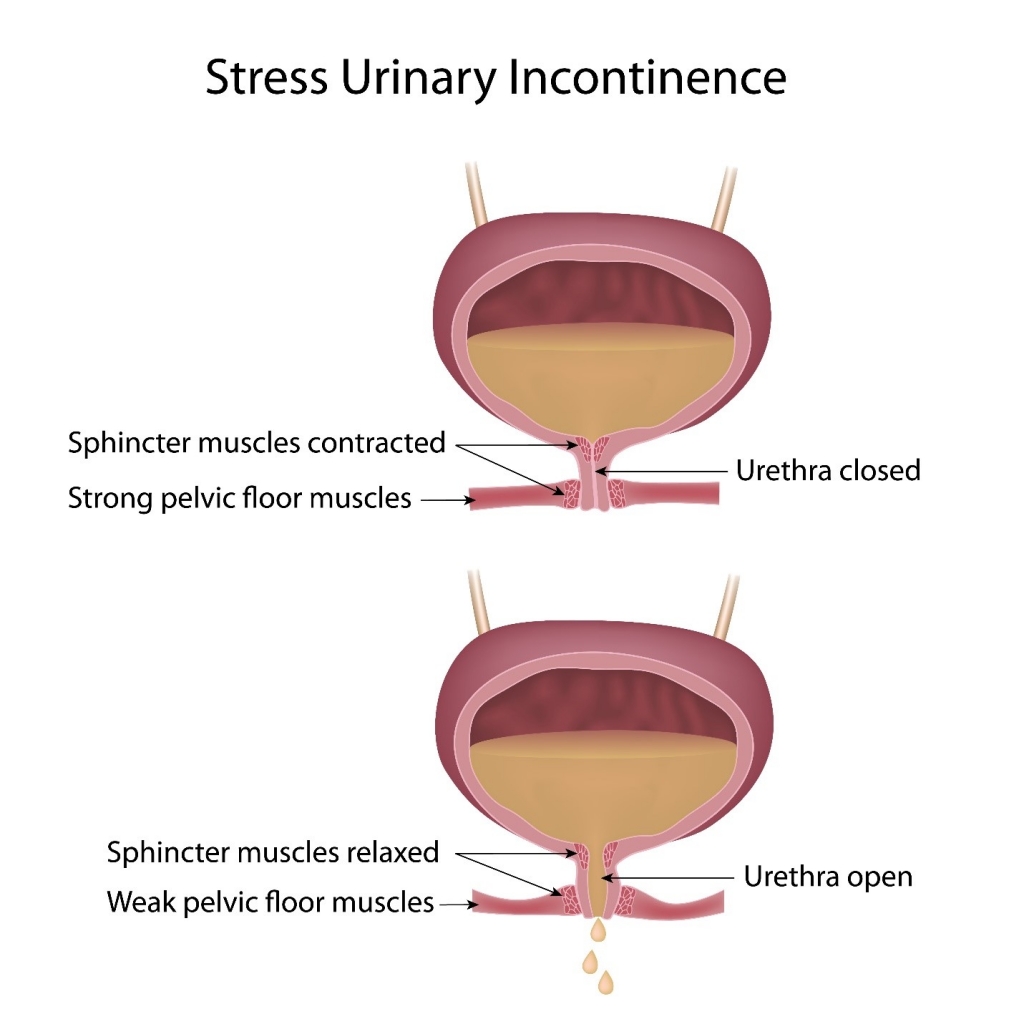
Urinary incontinence (UI) is the loss of bladder control that causes urine leakage.
There are several types and possible causes of UI. Sometimes it’s caused by damage to the nerves of the bladder or other parts of the nervous system. Sometimes it develops when the urethra becomes blocked. Or, it may be caused by medication side effects that make it difficult to reach the bathroom in time.
Most often, though, UI is caused by weak pelvic floor muscles. Part of the larger core muscle system, the pelvic floor muscles act as a “sling” that stretches across the pelvis and holds the bladder, bowel, uterus, and vagina firmly in place. These muscles often become stretched and weakened after pregnancy and childbirth. They can also weaken because of hormonal changes during menopause that alter tissue and muscle strength.
Weak pelvic floor muscles can lead to pelvic organ prolapse, which is when an organ (such as the uterus) slips from its normal position in the pelvis and presses on another organ (such as the bladder).
Pelvic organ prolapse is a common cause of stress urinary incontinence, the leading type of UI in women.
In addition to urine leakage, pelvic organ prolapse symptoms can include:
- A chronic feeling of urgency to urinate
- Painful urination
- A feeling of fullness or pressure in the pelvic region
- A feeling that something is pressing on or falling out of the vagina
- Low back pain
- Vaginal spotting or bleeding
- Pain during sex
- Bleeding after sex
Women often ask, “How do I know if my prolapse is severe?” If you have a mild prolapse, you may not experience symptoms at all. If you have a more severe prolapse, you’ll probably know something isn’t quite right. You might feel a bulging sensation in the vagina or have a feeling of heaviness in the pelvis—these are telltale signs of a moderate prolapse. In severe cases, the uterus or cervix can actually protrude out of the vagina.
All women—regardless of age—should do regular Kegel exercises to keep the pelvic floor muscles strong, which can help prevent or even reverse mild prolapse.
Managing UI Is Costly—in More Ways Than One
Dealing with UI can be costly, both financially and psychologically. It can seriously impact your quality of life. Yet, many women never seek treatment, assuming that incontinence is a normal part of life.
If you suffer from UI, managing it can be more than a hassle. You might avoid drinking water and other liquids while away from home. You might wear black “just in case” of an accident or carry around bulky, uncomfortable bladder pads. You might avoid intimacy with your partner or put off traveling and doing things you love out of fear of not having constant access to a bathroom. All of this can feel very disempowering.

And then there are the financial costs:
- In Australia, the total cost for UI treatment (women and men) in 2010 was $270.8 million. This included hospital costs, visits with specialists, general practitioners, and allied health professionals, and costs for pharmaceuticals, medical imaging, and research. It didn’t include out-of-pocket costs for over-the-counter products and continence aids, which were also likely high.2
- In the U.S., the most recent estimate of the annual direct costs of incontinence for women was more than $16 billion—more than the direct costs of breast, ovarian, cervical, and uterine cancers combined.3
- Routine care costs for things like absorbent pads, laundry, and continence aids are also significant. A U.S. study found that women with severe incontinence pay around $900 a year for routine care alone.3
Perhaps the biggest cost of UI, though, is the impact on quality of life.
One study found that urinary incontinence is one of four conditions (which also include Alzheimer’s disease, arthritis, and the effects of stroke) that has the most adverse impact on health-related quality of life—more than diabetes, heart disease, and asthma.4
Ladies: UI is common, but it’s not a normal part of aging.
Treatments for UI and Prolapse
It’s important to know that bladder leakage is not normal—even if it’s just a few drops when you laugh, cough, or sneeze. If you’re among the one in three women who experience bladder leaks, there are treatments that can help. UI does not have to dominate what you do or where you go or your intimacy with your partner.

Possible treatments for women with stress UI include:
- Pelvic floor exercises: Physiotherapists recommend strengthening the pelvic floor muscles with regular Kegel exercise as your first line of defense against UI. If you’ve had a baby, your OB-GYN has probably already counseled you on the importance of doing Kegel exercises. If not, it’s never too late to start. Doing Kegels regularly can help you prevent or reduce leaks from stress UI. You can do Kegels anytime, anywhere—at your desk at work, at home in bed, or even while standing in line. To minimize distractions, though, it’s best to set aside time to do them at home, preferably with a pelvic floor exerciser like PeriCoach.
- Pessary: Your doctor may recommend a pessary device, which is inserted into the vagina and helps reposition the urethra (the tube that carries urine from the bladder out of the body); a pessary can help reduce urine leakage.
- Injectable bulking agents: Your doctor may recommend injections to strengthen the urethral wall, which can help reduce or eliminate leaks; this option is generally limited to women whose stress incontinence has caused problems with the urethra.
- Pelvic organ prolapse surgery: In cases of severe prolapse, surgery may be necessary. There are five types of pelvic organ prolapse involving different organs: the bladder (cystocele), intestines (enterocele), rectum (rectocele), uterus (uterine prolapse), and vagina (vaginal vault prolapse). Pelvic organ prolapse stages range from mild (stage 1) to severe (stage 4). Which surgery is appropriate depends on which organs are affected, but it usually involves repositioning the prolapsed organ(s) and securing connective tissues.
In some cases, Kegel exercises alone can help strengthen the pelvic floor muscles enough to prevent leaks. The key is doing them regularly and doing them correctly. Not sure how to correctly Kegel? Check out this guide to Kegel exercises for women with urinary incontinence. We also recommend using a pelvic floor exerciser with real-time biofeedback, like PeriCoach. In fact, two out of three women using PeriCoach are able to improve their ‘Kegel technique’ which leads to improvement in strength, less leaks and enhanced sexual satisfaction
Get the Conversation About UI Started
UI and pelvic organ prolapse are extremely common problems for women around the world. Sadly, they have not gotten the attention they truly deserve, in part because of the stigma still surrounding women’s sexual and reproductive health.
Many women are embarrassed to talk about issues like bladder leaks or painful sex—even with their doctors. PeriCoach wants to help change this. Our goal is to empower women with tools and information they need to take charge of their pelvic health. UI and prolapse are medical conditions that warrant the same attention as other health problems.
If you’re experiencing urine leakage, whether it’s a few drops when you strain or a stream, don’t wait—talk with your doctor.
About PeriCoach

PeriCoach is an innovative Kegel biofeedback device that guides you through Kegel exercises. The device pairs with your smartphone (via Bluetooth) and sends data to your phone as you squeeze against it. This allows to you see your progress in real time!
Doctors and physiotherapists recommend PeriCoach for their patients, and clinical evidence shows its effectiveness. A robust randomized clinical trial involving women with (predominantly) stress UI found that those who used PeriCoach as part of their clinician-guided pelvic floor rehabilitation program had statistically significant improvements in quality of life and sexual function.
Regular exercise with PeriCoach can help you strengthen your pelvic floor muscles over time—and strong muscles can help prevent or even reverse stress UI.
Try the PeriCoach 8-Week Challenge and hear what real women are saying about how PeriCoach has changed their lives.
Sources:


