Ladies, your body is a marvel. Trillions of processes go on inside your brain, cells, and gut every minute of every day to keep your body running like a fine-tuned machine. Then there are your muscles, which convert energy into motion and keep blood flowing through your body.
Which brings us to our main topic: your pelvic floor. Both men and women have pelvic floor muscles, but this article is all about pelvic muscles in females.
What Is the Pelvic Floor?
The pelvic floor is a system of muscles, ligaments, and connective tissues that stretches across your pelvis and holds up your pelvic organs. Picture it like a sling or hammock that connects to each side of your pelvis and keeps your uterus, bladder, and bowel snugly in place.
Several things can weaken your pelvic floor muscles. In fact, one in three women will experience bladder leakage, known urinary incontinence (UI), at some point. When you’re pregnant, the baby puts stress on your pelvic floor—so does the strain of childbirth. Hormonal changes during menopause can also weaken your pelvic floor. So can carrying extra weight.
When your pelvic floor is weak, an organ inside your pelvis can slip from its normal position. This is called pelvic organ prolapse, and it can cause problems like bladder leaks.
Sadly, only around half of women tell their doctors about pelvic floor problems. This has led to an epidemic of silent suffering. If you leak urine, or if something just doesn’t feel right, talk to your doctor. There are solutions.
A brief anatomy lesson can help you make sense of how the pelvic floor works. Don’t worry, we’ll try to make it quick and painless!
Pelvic Floor Anatomy: An Inside Look
Your pelvic floor muscles are part of your core. They help you maintain good posture and intra-abdominal pressure, which keeps your pelvic organs right where they should be when you cough, laugh, or sneeze.
Your pelvic floor muscles also affect sexual pleasure—most women don’t know that weak pelvic floor muscles can reduce pleasure during sex.
Earlier we said the pelvic floor acts like a sling. When viewed vertically, it looks more like a funnel of thin but strong muscles that close off the pelvic cavity from below. The levator ani and the coccygeus are two important pelvic floor muscles:
- The levator ani is actually a sheet of several muscles that attach to a triangular bone called the sacrum at the base of the spine.
- The coccygeus is a smaller muscle that sits behind the levator ani.
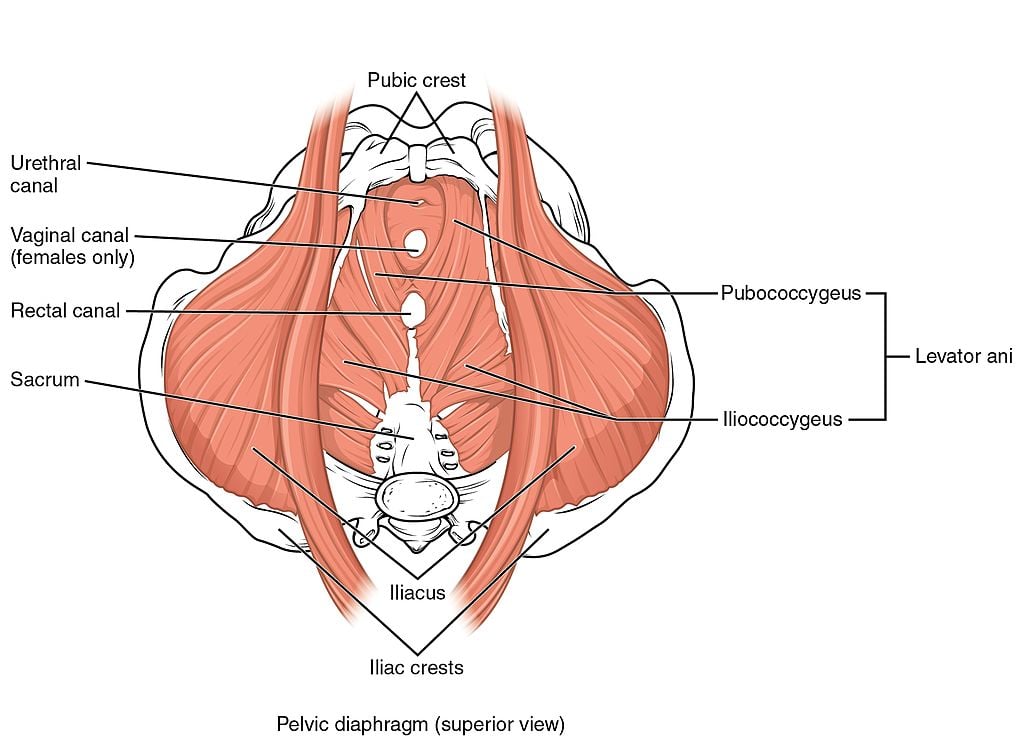
These muscles are important because they support all the organs in your pelvis and help you maintain fecal continence. Another important one is the pubococcygeus, a muscle that controls urine flow. The levator ani and coccygeus form the pelvic diaphragm, which seals off your pelvic cavity.
But your pelvic floor isn’t completely sealed off. There are natural gaps between your muscles called hiatuses that allow organs to pass through. Your urethra, for example, passes through one of these gaps to carry urine from your bladder to the outside your body.
Enough pelvic floor muscle anatomy for one day!
Preventing Bladder Leaks
If you leak urine or have trouble getting to a bathroom in time, there are things you can do to improve your symptoms. This is true regardless of your age or how many children you’ve had. You don’t have to live with bladder leaks.

These things can help:
- Doing Kegel exercises: Doing Kegels regularly will help you build up your pelvic floor strength over time. Stronger muscles can reduce your chance of bladder leaks or improve symptoms you already have. Stronger muscles can also lead to heightened pleasure during intercourse and even longer, stronger orgasms.
- Avoiding certain beverages: If you have trouble making it to the bathroom in time (urge incontinence) or if you leak urine when you cough, laugh, or sneeze (stress incontinence), following a fluid intake schedule can help you avoid these issues. Also avoid things that can irritate your bladder, like caffeinated and carbonated beverages, and alcoholic drinks.
- Making healthy lifestyle changes: Losing weight can help improve bladder symptoms, since extra weight puts more pressure on your pelvic floor. Quitting smoking is also important; smoking can degrade your muscle fibers and cause coughing, both of which can cause pelvic floor weakness. If you have a chronic cough, get treatment.
You can do all these things right away. Kegels are a great place to start.
The PeriCoach Kegel exerciser can help you target the right muscles. PeriCoach is a vaginally insertable device designed exclusively for women. It has three built-in biofeedback sensors that detect when you squeeze against the device.
PeriCoach pairs with your smartphone via Bluetooth and guides you through the exercises in real time! You can see your progress each time you squeeze and release.



