Understanding the Comorbidities Associated with Urinary Incontinence
It’s well accepted that pregnancy, childbirth and menopause are all common causes of urinary incontinence, however, it is easy to overlook other comorbidities that also affect the severity and likelihood having incontinence. Medical conditions such as diabetes, obesity and pulmonary disorders increase the likelihood of having urinary incontinence. Not to mention the physical and psychological impacts urinary incontinence has on a person.
The comorbidities seen in older persons with UI are generally chronic diseases such as diabetes mellitus or cardiovascular disease, with onset in later adulthood. But patients with UI may have neurological comorbidities such as multiple sclerosis, spinal cord lesions or injuries, or genitourinary comorbidities such as recurrent, symptomatic urinary tract infections.[i]
As if suffering from any chronic illness isn’t bad enough, if you are a woman who also suffers with urinary incontinence, the blow can be twice as hard. The extra force exerted onto the pelvic floor by a chronic cough, or carrying excess weight, wreaks havoc on a bladder leakage problem. Plus, in a twist of irony, in some cases, the very thing that could help ease their medical condition – exercise — is being avoided due to the embarrassment and discomfort caused by leaking urine.
Professor Chantale Dumoulin, Ph.D., recently noted that women with osteoporosis are at risk for incontinence because fractures of the lumbar spine can make them slump, putting more pressure on the pelvic floor. Exercise actually helps in the treatment of osteoporosis, but those with incontinence who are prone to leaking urine when physically active, are deterred from exercising[ii]
General practitioners should discuss the presence of urinary incontinence in patients with the described comorbidities, so as to be able to offer appropriate treatment/management options or referrals.
Dr. Leslie Rickey, Yale, MPH, MD, highlights both the physical and psychological impacts of urinary incontinence, noting that many of the same conditions that increase the likelihood of incontinence such as diabetes, obesity and pulmonary disorders, can actually also be caused or worsened by incontinence. As Dr. Rickey says, “women start leaking and stop exercising leading into a downward spiral which affects overall wellness and health.”
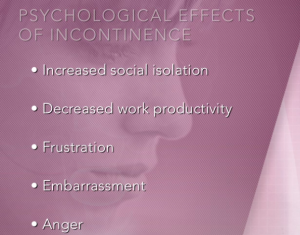
The psychological effects of urinary incontinence can be equally as damaging. Frustration and embarrassment can lead to increased social isolation, decreased work productivity and an overall effect on mood commonly causing anger or depression.
All of this can have a significant negative impact on women’s lives. They may avoid participating in their favorite sport or even leaving the house due to the risk of urine leakage. Urinary incontinence can also result in negative body image and/or reduced self esteem[i]
Treating incontinence therefore, has far greater reaching outcomes than could be anticipated- reducing the burden of cost to society by not having to pay for treatment of chronic illnesses and ensuring a greater number of women are in productive employment, and perhaps more importantly, ensuring that not only women’s physical, but mental wellbeing is optimized.
Watch Dr. Rickey discuss more about the effects of urinary incontinence and how the PeriCoach can help!
To read more about osteoporosis and incontinence click here.
[i] http://www.womhealth.org.au/conditions-and-treatments/urinary-incontinence-fact-sheet
[i] https://www.researchgate.net/publication/9016166_Risks_comorbidities_complications_and_quality_of_life_in_patients_with_urinary_incontinence
[ii] https://well.blogs.nytimes.com/2016/02/24/treating-incontinence-in-women-with-osteoporosis/?_r=2